Assessment of relationship between the use of household products and atopic dermatitis in Seoul: focused on products with associated risks
Article information
Abstract
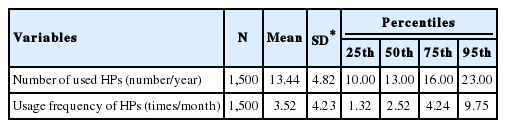
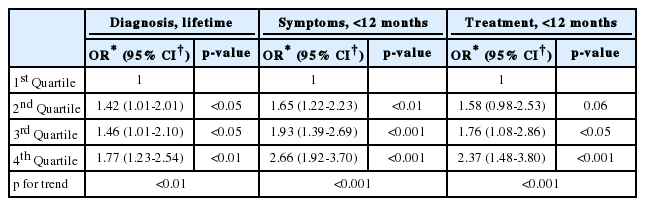
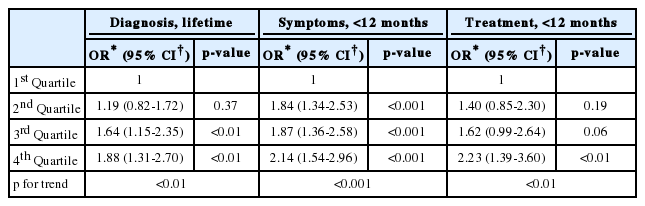
The purpose of this study was to evaluate the relationship between the use of certain household products (HPs) at home and atopic dermatitis (AD) in adults. The study was conducted on 1,500 households in Seoul, South Korea. We obtained information on general characteristics, the use of HPs, and AD through an online panel survey in July 2018. HPs were selected as 23 kinds of products with associated risks that are management targets of the Ministry of Environment. The international study of asthma and allergies in childhood was used for the AD questionnaires. Logistic regression analysis was used to identify AD affected by the use of HPs. Average number of used HPs was 13.44 out of 23, and average usage frequency of HPs was 3.52 times a month at home in Seoul for the last 1 year. Compared with subjects with a low number of HPs used (reference), subjects with a high number of used HPs (4th quartile) were more likely to have lifetime diagnosis of AD (odds ratio (OR) = 1.77, 95% confidence interval (CI); 1.23-2.54), symptoms of AD in the last 12 months (OR = 2.66, 95% CI; 1.92-3.70), and treatment of AD in the last 12 months (OR = 2.37, 95% CI; 1.48-3.80). Compared with subjects with a low HPs usage frequency (reference), subjects with a high HPs usage frequency (4th quartile) were more likely to have lifetime diagnosis of AD (OR = 1.88, 95% CI; 1.31-2.70), symptoms of AD in the last 12 months (OR = 2.14, 95% CI; 1.54-2.96), and treatment of AD in the last 12 months (OR = 2.23, 95% CI; 1.39-3.60). Therefore, the use of HPs was significantly associated with AD. The findings of this study might be useful as basic data for managing allergic diseases and establishing preventive measures.
INTRODUCTION
Household products (HPs) are constantly being used in daily living, to the extent that a new phrase “homo chemicus” has been coined, meaning humans living in a state of dependence on chemical products [1]. Since the humidifier disinfectant accident in 2011, awareness of the risk of HPs has grown, as incidents involving chemicals in HPs continue to occur, such as the inclusion of humidifier disinfectants in some toothpastes, the presence of pesticide in eggs, the discovery of hazardous substances in sanitary napkins, methanol from vehicles in washers, and radon in beds [2]. In fact, according to the Korea Consumer Agency (KCA), 1,529 cases of the risks of HPs were received through consumer surveillance system in the 3-year period from 2014 to 2016, with 46.5% more cases in 2016 than in 2014 [3].
HPs are continuously produced according to the purpose and use of each manufacturing company, and there are many chemicals in these HPs that are not properly managed [4]. According to the National Institute of Environmental Research (NIER), 682 products, which account for about 50% of the 1,369 HPs in total, were reported as using nanomaterials [5]. In the study of ingredients and hazardous substances contained in detergents and disinfectants, 38 of the 163 ingredients were classified as dangerous substances, and some of them have been shown to be harmful or carcinogenic in oral, transdermal, and inhalation exposure [6]. In an overseas study, 133 kinds of volatile organic compounds were detected among 25 HPs such as laundry products, personal products, cleaning products, and fragrances [7]. In addition, since there are still cases in which the labeling of product ingredients is insufficient, consumers may not be properly informed of the harmful chemical substances contained in HPs, as was the case in the humidifier disinfectant incident, and may be exposed to unexpected health effects [8].
A previous study has reported that chemicals in HPs can adversely affect health, resulting in symptoms such as skin rash, allergies, eye irritation, and dyspnea [9]. Of these, atopic dermatitis (AD) with severe itching and dry symptoms is one of the most common skin diseases not only for infants and children but also for adults in Korea [10], and the prevalence of AD continues to grow with the rapid increase of allergic diseases worldwide [11]. According to Statistics Korea (KOSTAT), rates of AD diagnosis in adults aged 19 and over increased from 2.4% in 2007 to 4.1% in 2017 [12]. The cause of AD has not yet been clearly identified, but it is known that various environmental or genetic factors interact with each other and contribute in a complex manner [13]. Significantly, it has been reported that environmental factors are related to the increase of exposure to antigens due to Korea’s westernization and changes in the living environment, as well as the presence of allergens such as automobile exhaust, dust, particle matter, etc. [14].
While studies on adult AD continue to be conducted abroad [15], there has been a lack of interest in adult AD in Korea compared to children AD. As such, the purpose of this study is to identify usage status of HPs at home in Seoul, targeting products with associated risks that are management targets of the Korean Ministry of Environment (ME), and to evaluate the relationship between the use of HPs and AD in adults.
MATERIALS AND METHODS
Study Population
An online survey was conducted on 1,500 households who lived in Seoul for more than 1 year, using online participants who voluntarily registered with a survey company for 20 days from July 11 to July 30, 2018. To ensure that the survey sample was representative of households in Seoul, we used the statistical data of the Population and Housing Census in 2015, and applied population proportional allocation according to the 5 major areas of Seoul and type of residence. The subjects were limited to adults aged 19 and over. This study was approved by the Institutional Review Board of Seoul Medical Center (IRB no. 2018-05-006).
Survey
As of early July 2018, 191,850 out of 283,685 participants in the Seoul registered survey company were randomly extracted and sent e-mail requesting participation through an email program. 25,285 out of 191,850 subjects confirmed via e-mail, and 5,934 of them accessed the online survey. However, 656 subjects were excluded through the screening, 3,424 subjects were excluded due to over-representation of proportional allocation, and 156 subjects were excluded due to abandonment, thus only 1,698 subjects completed the survey. Of these, 198 subjects who repeatedly responded to a certain interval or had a short response time were excluded. Ultimately, 1,500 subjects were included in the analysis. Since the subjects are panel members managed by the survey company, they paid for itself in the form of mileage to the subjects.
General Characteristics
The general characteristics of survey included the following: gender (male, female), age (20-29 years, 30-39 years, 40-49 years, ≥50 years), area (downtown, northeast, northwest, southeast, southwest), residence period (1-3 years, 3-5 years, ≥5 years), residence type (detached house, apartment, multiplex house, commercial house), marital status (single, married), education (≤high school, university, ≥graduate school), occupation (production, professional, office work, sales/service, self-employed, student, housewife, unemployed), monthly household income (<2 million won, 2-5 million won, 5-7 million won, ≥7 million won), number of residents (1 person, 2 people, 3 people, 4 people, ≥5 people), household type (1 generation, 2 generations, ≥3 generations, non-kin, 1 person), minor child (no, yes), residence scale (≤60 m2 , 60-85 m2 , 85-135 m2 , >135 m2 ).
The use of HPs at home
HPs were selected as 23 kinds of products with associated risks that are management targets of the ME [16]. Products with associated risks are classified as follows in accordance with standard guided by ME: 5 kinds of detergents (cleaner, synthetic detergent, bleaching agent, softening agent, windshield washer fluid), 6 kinds of coatings/adhesives (coating, rust inhibitor, anti-fogging agent, adhesive, ironing auxiliaries, niche filler), 2 kinds of aromatic products (air freshener, deodorant), 3 kinds of dyes (object decolorant and dye, tattoo dye, printing ink and toner) 4 kinds of biocidal products (disinfectant, insect repellent, preservative, algicide), 3 kinds of others (candle, desiccant, antifreeze). In the survey, the use (used, not used) and usage frequency (1-11 times a year, 1-3 times a month, 1-6 times a week, 1-4 times a day) of each product for the last 1 year were examined. If the subject used the product more than 4 times a day, they were asked to fill in the number directly. Usage frequency of each product was quantitatively converted to a per month figure.
Status of AD
The status of AD was assessed using the International Study of Asthma and Allergies in Childhood questionnaires. The survey included the following information related to AD, indoor environmental factors, and family history: lifetime diagnosis of AD (no, yes), symptoms of AD within the last 12 months (no, yes), treatment of AD within the last 12 months (no, yes), current smoking (no, past experience, yes), indoor secondhand smoking (no, 1-2 times a week, 3-4 times a week, 5-6 times a week, everyday), remodeling in the last 12 months (no, yes), use of new furniture in the last 12 months (no, yes), mold stain in current residence (no, yes), pets in current residence (no, yes), parental lifetime diagnosis of allergic diseases (no, yes).
Statistics
The number of used HPs was represented by the total number of HPs who answered that they use each product, and usage frequency was expressed as arithmetic mean and standard deviation (SD) using average usage frequency for each product. These were divided into quartiles in the analysis of AD. General characteristics, indoor environmental factors, family history, and number of used HPs and usage frequency were subjected to a Chi-square test. To assess the relationship between the use of HPs and AD, logistic regression analysis was conducted after correcting for general characteristics, indoor environmental factors, and family history of this study. These results were shown by odds ratio (OR) and had a 95% confidence interval (CI). All of the statistics were performed using Statistical Analysis Software (SPSS version 18.0, SPSS Inc.).
RESULTS
Usage Status of HPs
Average number of used HPs and average usage frequency of HPs of 1,500 households in Seoul were 13.44 out of 23 and 3.52 times a month, respectively (Table 1). Frequency distribution of number of used HPs are presented in Table S1. When the use of HPs was divided into quartiles, the number of used HPs was ≤10 in the 1st quartile, 11-13 in the 2nd quartile, 14- 16 in the 3rd quartile, and ≥17 in the 4th quartile, and the usage frequency was ≤1.32 times a month in the 1st quartile, 1.32-2.52 times a month in the 2nd quartile, 2.52-4.24 times a month in the 3rd quartile, and >4.24 times a month in the 4th quartile.
Related Factors of AD
Table 2 showed general characteristics, indoor environmental factors, family history, and the use distribution of HPs of the subjects according to AD. The percentage of adults with the experience of AD diagnosis in their lifetime was significantly higher than those without, as follows: 28.8% for those aged 20-29 years (p<0.05), 48.3% for those who were single (p<0.05), 18.8% for those who had a history of smoking (p<0.05), 22.1% for those with daily indoor secondhand smoke exposure (p<0.01), 32.6% for those who had remodeled in the last 12 months (p<0.001), 61.7% for those with mold stain in the current residence (p<0.001), 23.3% for those with pets in the current residence (p<0.001), 45.7% for those with a parental lifetime diagnosis of allergic diseases (p<0.001), 29.8% for number of used HPs in the 4th quartile (p<0.001), 32.6% for usage frequency of HPs in the 4th quartile (p<0.001). Adults with the experience of symptoms of AD within the last 12 months were significantly higher than those without the experience of AD in the following groups: 52.9% for females (p<0.05), 14.7% for ≤high school graduation (p<0.05), 20.9% for those with a residence size ≤60 m2 (p<0.05), 24.1% for those with daily indoor secondhand smoke exposure (p<0.001), 31.8% for those who had remodeled in the last 12 months (p<0.001), 38.8% for those with new furniture in the last 12 months (p<0.001), 59.9% for those with a mold stain in their current residence (p<0.001), 20.2% for those with pets in their current residence (p<0.05), 38.8% for those with a parental lifetime diagnosis of allergic diseases (p<0.001), 26.6% for number of used HPs in the 4th quartile (p<0.001), 29.6% for usage frequency of HPs in the 4th quartile (p<0.001). Adults with the experience of treatment of AD within the last 12 months were significantly higher than those without in the following groups: 21.2% for those with graduate school education or higher (p<0.05), 26.0% for those with a household income of 7 million won per month or more (p<0.05), 12.5% for those with a residence less than 135 m2 (p<0.01), 23.8% for those with everyday indoor secondhand smoke exposure (p<0.05), 37.7% for those who had remodeled in the last 12 months (p<0.001), 44.2% for those that had used new furniture in the last 12 months (p<0.001), 64.1% for those with a mold stain in their current residence (p<0.001), 27.7% for those with pets in their current residence (p<0.05), 55.8% for those with a parental lifetime diagnosis of allergic diseases (p<0.001), 37.3% for number of used HPs in the 4th quartile (p<0.001), 37.7% for usage frequency of HPs in the 4th quartile (p<0.001).
Relationship Between Number of Used HPs and AD
In order to evaluate the relationship between the number of used HPs and AD, a logistic regression analysis was performed by adjusting the confounding variables. The results are shown in Table 3. The risk of lifetime diagnosis of AD compared to the 1st quartile was 1.42 times higher (95% CI; 1.01-2.01) in the 2nd quartile, 1.46 times higher (95% CI; 1.01-2.10) in the 3rd quartile, and 1.77 times higher (95% CI; 1.23-2.54) in the 4th quartile. The risk of symptoms of AD within the last 12 months was 1.65 times higher (95% CI; 1.22-2.23) in the 2nd quartile, 1.93 times higher (95% CI; 1.39-2.69) in the 3rd quartile, and 2.66 times higher (95% CI; 1.92-3.70) in the 4th quartile. The risk of treatment of AD within the last 12 months was 1.76 times (95% CI; 1.08-2.86) higher in the 3rd quartile, and 2.37 times higher (95% CI; 1.48-3.80) in the 4th quartile. As the number of used HPs increased, the risks of lifetime diagnosis (p<0.01), symptoms within the last 12 months (p<0.001), and treatment of AD within the last 12 months (p<0.001) were increased significantly.
Relationship Between Usage Frequency of HPs and AD
As shown in Table 4, a logistic regression analysis was performed after adjusting for confounding variables to evaluate the relationship between the usage frequency of HPs and AD. Compared to the 1st quartile, the risk of lifetime diagnosis of AD was 1.64 times higher (95% CI; 1.15-2.35) in the 3rd quartile, and 1.88 times higher (95% CI; 1.31-2.70) in the 4th quartile. The risk of symptoms of AD within the last 12 months was 1.84 times higher (95% CI; 1.34-2.53) in the 2nd quartile, 1.87 times (95% CI; 1.36-2.58) higher in the 3rd quartile, and 2.14 times higher (95% CI; 1.54-2.96) in the 4th quartile. The risk of treatment of AD within the last 12 months was 2.23 times higher (95% CI; 1.39-3.60) in the 4th quartile. As usage frequency of HPs increased, the risk of lifetime diagnosis (p<0.01), symptoms within the last 12 months (p<0.001), and treatment within the last 12 months (p<0.01) of AD was increased significantly. These results had a similar trend to the number of used HPs. Relationships between usage of 23 individual HP and AD are presented in Table S2.
DISCUSSION
This study of average number of used HPs and average usage frequency at home in Seoul for the last 1 year showed that consumers are still highly dependent on HPs. According to risk information trend analysis of household chemical HPs of KCA, accidents such as eye damage, internal dangerous substances, poisoning, burns, and pain at home were the most frequent type when risk was broken down by location [3]. This is thought to be related to the high use rates of HPs at home.
The experience rates of lifetime diagnosis of AD, symptoms of AD within the last 12 months, and treatment of AD within the last 12 months in this study were higher than in a previous study [10]. This is because not only physical factors but also psychological factors such as stress and depression are reported to be involved in the onset of AD [17]. It is thought that those factors affect the continuous increase of experience rates of AD.
In this study, AD was found to be associated with gender, age, marital status, education, household income, residence scale, smoking, indoor secondhand smoking, remodeling in the last 12 months, the use of new furniture in the last 12 months, mold stain, and parental lifetime diagnosis of allergic diseases. Previous studies on adults have reported the association of AD with gender, age, marital status, education, household income, number of residents, and residential area [17,18], and the direction of relevance was consistent with this study. In particular, AD was significantly associated with parental family history [19], showing similar trend in this study. In addition, AD is also reported to be influenced by obesity, smoking, drinking, pets, stress, and dietary habits [20-23].
The findings of this study, which analyzed the relationship between the use of HPs and AD, shows that the risk of lifetime diagnosis of AD, symptoms of AD within the last 12 months, and treatment of AD within the last 12 months was significantly increased as the number of used HPs and their usage frequency increased. It has been reported that surfactant or antimicrobial components contained in HPs cause allergy from skin contact and increase the risk of developing AD when it exposes continuously [24,25,26], and this study supports this finding. In immunological mechanisms, harmful chemicals contained in HPs are exposed to antigens and the balance between T-helper type 1 (Th1) and T-helper type 2 (Th2) cytokine is broken, resulting in overproduced Th2 cytokines such as interleukin (IL)-4, 5, 9, 13 stimulating B cells and increasing immunoglobulin E (IgE) [27]. Increased IgE binds to receptors on the surface of mast cells and secretes chemicals such as histamine, stimulating blood vessels and skin which leads to AD [28]. In a previous domestic study, the risks of skin eczema were significantly increased according to usage frequency of antibacterial housewares, as follows: by 1.13 times (95% CI; 1.04-1.24) in the 2nd quartile, by 1.15 times (95% CI; 1.05-1.26) in the 3rd quartile, and by 1.13 times (95% CI; 1.03-1.24) in the 4th quartile [29]. In an overseas study conducted through an online survey, 66.8% of the population was exposed to HPs at least 1 time a week due to the use of HPs, and 4.8% of them experienced skin symptoms [30]. A study of the effects of the use of disinfectants at home on allergic diseases found that the risk of AD was significantly higher when disinfectants were used, as follows: 2.6 times higher (95% CI; 1.2-5.6) for lifetime symptoms of skin eczema, 7.0 times higher (95% CI; 1.8-27.1) for symptoms of skin eczema within the last 12 months, and 2.5 times higher (95% CI; 1.1-6.0) for lifetime symptoms of skin rash [31].
This study has a limitation in that it can be interpreted that there is the possibility of underestimation, because it includes subjects who responded that they did not use HPs in their usage frequency of HPs. In addition, the subjects responded to questionnaire relied on his or her memory to answer the online survey, so there is a possibility that the results are affected not only by reliability but also by recall bias. Nevertheless, the subjects of this study were applied population proportional allocation to represent households in Seoul, and this study shows that the risk of AD in adults was significantly increased as the number of used HPs and their usage frequency increased. Therefore, the findings of this study might be useful as basic data for managing allergic diseases and establishing preventive measures.
Acknowledgements
The authors thank Seoul Medical Center Research Institute, “A study on the use and exposure of hazardous substances contained in consumer products in the household, 2018 (18-A05)”.
Notes
The authors have no conflicts of interest to declare in relation to the material presented in this paper.
Funding
This study was supported by Seoul Medical Center Research Institute, Republic of Korea